What is the tricuspid valve?
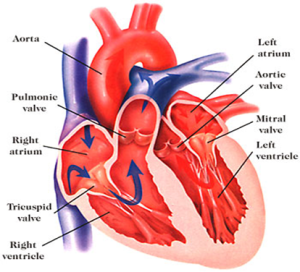
The heart consists of four heart valves. Two of them are on the left side and the other two are on the right side. The tricuspid valve is the inlet valve of the right side of the heart and is located between the two chambers. The tricuspid valve allows unobstructed flow of blood into the pumping chamber (right ventricle) of the heart without any resistance.
Unlike the mitral valve, the tricuspid valve has three triangulated doors (leaflets) on the frame(annulus) and is held in place with strings allowing doors to open only one way ensuring blood flow only in a forward direction. If the strings break or get loose, or the frame gets bigger,this leads to formation of gaps between the doors which causes leakage or backward flow. This can also occur if the doors get damaged due to infection.
When the tricuspid valve becomes diseased, infected or malfunctions, it needs to be repaired or replaced with an artificial heart valve or other available alternatives.
Types of tricuspid valve disease
It is quite uncommon for the tricuspid valve to become faulty on its own unless the patient has developed severe infection. Most commonly, tricuspid valve disease is the end result of the other valve diseases or lung diseases.
Tricuspid valve malfunction can result from mainly two mechanisms
- Tricuspid Stenosis – In this disease, the opening of the tricuspid valve is restricted due to structural problems with the valve or surrounding tissues. Typically, the common causes for this condition are secondary to infection like rheumatic fever, or rare tumours.
- Tricuspid regurgitation – in this disease, the tricuspid valve does not close effectively leading to blood flowing backwards(leakage). The common cause for this type is due to outward stretch on the frame(annulus) of the tricuspid valve which causes a gap in the center of the valve causing it to leak. The other causes are bacterial infections(endocarditis), long standing atrial fibrillation, permanent pacemaker and a weak, enlarged heart.
When is the valve repaired or replaced?
Repairability of the valve depends on the causes of leakage, damage to the valve, complexity of surgery , patient choice and experience of the surgeon. In general, valve leakage secondary to a stretched frame is readily repairable in the hands of most surgeons, with very good long term results. If the leakage is secondary to bacterial infection then repairability depends on the damage caused by infection and experience of the treating surgeon. Problems due to rheumatic fever are difficult to repair and such repairs are undertaken by highly specialist surgeons.The majority of surgeons will elect to replace tricuspid valves diseased by rheumatic fever. Leakage due to long standing atrial fibrillation is readily repairable in most cases as the cause of leak is the stretched frame. Whatever the case may be, your surgeon will assess the valve after the repair and if not satisfied , your valve will be replaced with what you would have chosen prior to surgery.
Is valve repair better than replacement?
Valve repair is generally considered better than replacement. This is due to the fact that you retain your tissue which is resistant to infection, compared to an artificial heart valve. An artificial heart valve is a large foreign body implanted into your circulatory system which is in constant contact with blood. There is a risk of blood clot formation, which can cause artificial valves to fail. If a patient gets any blood infection, then there is a risk of an artificial heart valve getting infected, which requires major surgery to replace the valve. Both the risks above are significantly lower with valve repair. Valve repair also requires the use of artificial material but the quantity of that is much lower compared to artificial heart valves.
The other issue is the requirement of blood thinners like warfarin with artificial mechanical/metal valves. If you get a metal heart valve implantation then you need to be on warfarin for life, which is a strong blood thinner. It exposes patients to a life long risk of bleeding. With valve repair, patients do not need to take warfarin for life.
If a patient gets a tricuspid valve replacement with a tissue valve then he/she may not need to take warfarin. It is thought that tissue valves may last longer in the tricuspid position compared to other heart valves, but data is not robust. Nonetheless, tissue valves have a good record in the tricuspid position. Younger patients are very likely to outlive tissue valves which will definitely require reoperation or a procedure in future. Unlike this, a valve repair can last for many decades in the majority of patients.