Minimally invasive mitral valve repair
Different approaches for mitral valve repair/replacement
- Sternotomy – splitting the breast bone
- Minithoracotomy – minimally invasive approach via small incision on the right chest
Minimally invasive mitral valve surgery
This approach involves a 5-7 cm incision on the middle side of the right chest. There is another small incision in the right or left groin. The surgeon approaches the mitral valve via the space in between the ribs. The ribs are spread with the insertion of a retractor allowing the surgeon to have improved exposure of the heart. Another 5 mm incision is placed on the top of the chest to introduce a telescopic camera that assists the surgeon’s visualisation of the heart and mitral valve.
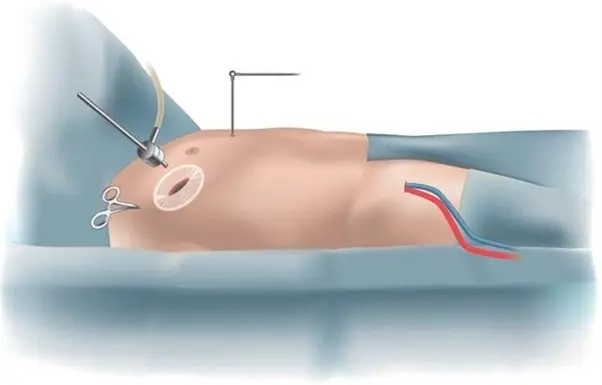
Incision in the groin is used to insert tubes in the heart to connect to the heart lung machine. The heart is stopped with a special solution. Valve is repaired or replaced depending on its condition. Heart is separated from the heart lung machine and allowed to beat normally on its own. At this stage, the anaesthetist and surgeon will assess the valve with an intra operative echocardiography to assess the valve function. Once satisfied, surgery will proceed in the usual manner to finish. Patient is transferred to the ICU still under anaesthetic.
If there are unexpected findings or difficulties, Dr Joshi will change the incision to a standard sternotomy incision to ensure your safety and good outcome. A good outcome is more important than incision. The occurrence of this event is quite uncommon.
What happens in the ICU?
Typically most patients are kept asleep with medications for 3-6 hrs to observe for stability. While you are asleep you will be breathing with a breathing machine. The ICU specialist (Intensivist) is in charge of your care while you recover in the ICU. When you wake up you will feel very sleepy and weak. You will notice a few lines , tubes and wires connected to you which are routine. You will feel a bit uncomfortable with all those attached to your body. These are removed as you progress in your care and most are removed by day 5. As a routine, you will be helped to get out of bed and sit in a chair for a few hours to help your lungs breathe better. A physiotherapist will take you for a short walk on day 2 in the ICU. The stay in ICU is typically for 2 days. You will be transferred to the cardiac ward for further care.
Will I be in a lot of pain?
Pain is very subjective. Pain from the chest wall incision is usually more severe than the incision on the breast bone. You will be on strong painkillers, some of which may have unpleasant side effects like nausea, vomiting and constipation. Nursing staff will manage your pain medication in close collaboration with you. You are encouraged to notify staff if your pain is unbearable, prevents you from deep breathing or keeps you awake.
Some patients may develop long term nerve pain that may result from the injury to nerves under the ribs. This is one of the downsides of this approach. Some patients may get fractures in the ribs that may take 6-8 weeks to heal.
Progress in the ward
You will be in a room once you arrive in the ward. You will be connected to a monitor so nurses can see any alarming signals from your heart rhythm. You need to be careful that the wires remain attached to your body properly. If they get detached, you should inform your nurse by pressing the call button. The most important thing in the ward is to start getting more mobile. You will be asked to walk 5 times every day and your physio will teach you exercises. You may have some wires connected to you which will be removed in the next few days. Removal of wires and lines are very tolerable. By day 5-7, you will be asked by physiotherapists to complete two flights of stairs. This is done to assess your fitness to be discharged home and your independent mobility. You will have a regular blood test and chest x rays. Electrolytes are frequently replaced with intravenous infusions.
Going home
Most patients are expected to be discharged between 5-7 days after minimally invasive surgery. You will receive discharge education from your nurse who will give you information about incisions, dressing, showering etc. A pharmacist will visit you to discuss your medications which might have changed a little bit. You must remember to take the discharge file with you that should include all your instructions regarding follow up appointments, a medication list and other material. You should carry this file with you when you visit your cardiologist or cardiac surgeon for follow up at 4-6 weeks.
Dressings
You will have a small dressing on the chest and one on the groin. You should remove it after 4 weeks under a running shower. You can remove it earlier if it starts to come off or breaks. If you have any concerns about the wound please visit your GP or notify Dr Joshi.
Follow up
You should arrange an appointment to see Dr Joshi in 6-8 weeks and your cardiologist in 8 weeks. You should visit your GP within a week after being discharged from hospital.
Advantages of minimally invasive approach:
Some of the advantages of a minimally invasive approach is reduced blood loss, shorter hospital stay and earlier return to activity. The breastbone (sternum) is kept intact which allows early resumption of activities like lifting weight or driving.
- Cosmetic – incision is small and in some patients barely visible
- Early recovery and return to activities
- Future reoperations on heart are less complicated if you need one
- Less blood loss, shorter ICU and hospital stay