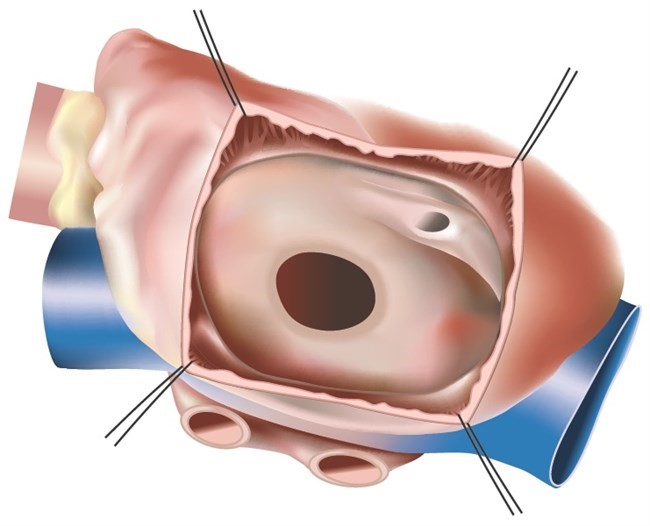
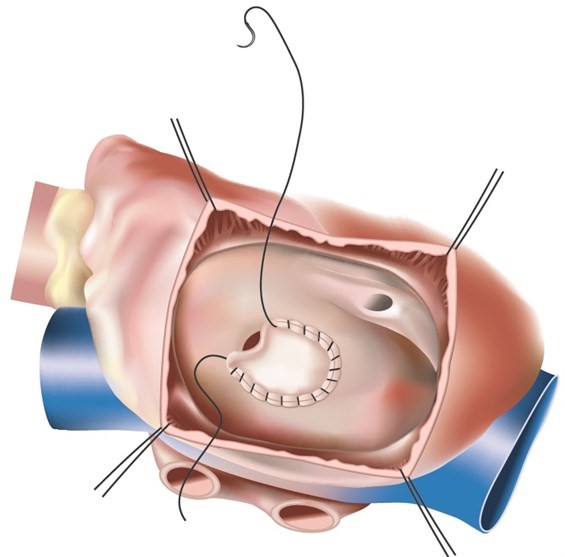
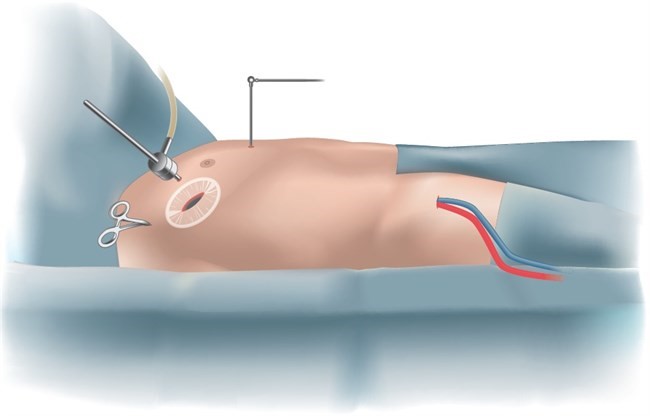
Minimally invasive closure of Atrial Septal Defect
An atrial septal defect (ASD) is a congenital heart defect where there is a hole in the atrial septum. The heart has two sides – right and left. The right side pumps unoxygenated blood to the lungs so blood can be oxygenated. The left side pumps oxygenated blood that it receives from lungs to the entire body. The two sides of the heart are separated by a tissue wall that ensures the blood does not mix between two sides. However, some people are born with defects in the wall allowing blood to flow between the two sides.
On each side of the heart there are two chambers. The chambers that collect blood are called the atrium and the chambers that pump blood out of the heart are called ventricles. The wall that separates the atrium is known as the atrial septum and the defect in this wall is called an Atrial Septal Defect(ASD). It can vary between 1 to 5 cm. We are all born with a small ASD at birth, but this usually seals off shortly thereafter. If the natural opening persists, it is called patent foramen ovale, the bigger opening is called ASD.
What are the symptoms of ASD?
ASD is quite often detected by accident. Symptoms typically include shortness of breath, fatigue, heart palpitations, or a decrease in exercise capacity. Patients usually have an audible heart murmur that is caused by the extra blood flow across the pulmonary valve to the lungs.
Is Is ASD potentially life threatening?
ASD causes excessive blood flow to the right side of the heart which can result in an enlarged right heart.This can then result in failure of the right heart and abnormal heart rhythms. Some patients can develop leakage of valves on the right side of the heart. The excessive blood flow in the right heart results in excessive blood flow in the lungs which in turn can damage vessels in the lung and causes life threatening complications like irreversible high pressures in lungs which can result in premature death or require heart lung transplantation.
When should an ASD be treated?
There are no rules but there is a general agreement that regardless of the age of the patient ASD should be treated. Some of the structural changes in the heart caused by an ASD over time are not entirely reversible. ASD closure before irreversible changes occur is therefore recommended. Most patients, children as well as adults, usually experience marked improvement of their symptoms after ASD closure.