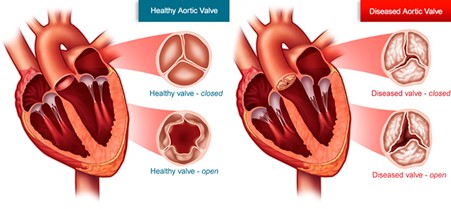
What is Aortic valve replacement ?
There are four heart valves. Two of them are on the left side and the other two are on the right side. Aortic valve is the outlet valve of the left side of the heart and is located at the beginning of the largest tube pumping blood from the heart that is known as the Aorta. When the aortic valve becomes diseased, infected or malfunctions it needs to be replaced with an artificial heart valve or other available alternatives. Surgery for replacement of aortic valve is known as aortic valve replacement – AVR
Hemisternotomy Aortic valve replacement & Right Anterior Thoracotomy Aortic Valve Replacement( RAT AVR)
Hemisternotomy Aortic valve replacement
What are the methods of Aortic valve replacement?
- AVR via full sternotomy (splitting breast bone)
- AVR via hemi sternotomy (splitting 1/3rd of breast bone by incision on 3rd rib)
- AVR via right anterior thoracotomy- RAT AVR (breast bone is not divided at all)
- AVR via transfemoral route (valve inserted via small incision in groin and no cuts on chest)
All the above methods of AVR are routinely employed. Except for AVR via full sternotomy the other three options are minimally invasive options for replacing aortic valve. Not splitting the breast bone (sternum) at all allows for quicker recovery, less blood loss, less hospital stay and better cosmesis.
Why hemisternotomy aortic valve replacement instead of other minimally invasive approach?
This is a minimally invasive approach without splitting the entire breast bone.
It is chosen as an approach in patients who have the following conditions :
- Heart and aorta located to the left of the breastbone(sternum) in which case other minimally invasive approach can be very difficult (RAT AVR)
- Patients who have big chest wall or significant muscles or fat on chest wall or women with large breasts where other key hole surgery like RAT AVR can become very challenging
- Women with breast implants where RAT AVR is not possible as it requires incision on the right side of chest wall and has significant potential to damage breast implants
- Patients who need other surgeries eg. Aorta repair
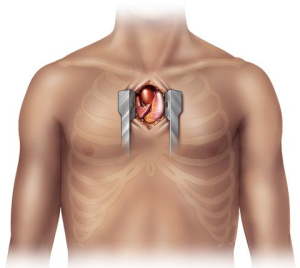
What is hemisternotomy ?
This is an approach where only the upper half of the breastbone (sternum) is divided. This allows the integrity of the chest wall due to intact lower sternum allowing for better recovery and early mobilization. The risks of sternal complications and bleeding may be lower with this approach.
The incision is 5-7 cm in the upper half of the chest and 1.5 cm incision in groin. The length of the incision in conventional valve surgery can range from 20-25 cm.
The heart is stopped and protected with a special chemical solution. Aortic valve is replaced with biological/tissue or mechanical valve depending on the patient’s choice and circumstances. After inserting the valve all incisions in the heart and skin are closed and the patient returns to ICU for a stay of 1-2 days. If there are any difficulties or complications during surgery, the incision will be extended to convert to full sternotomy as the safety of the patient takes priority over the incision.
What happens in the ICU ?
Typically most patients are kept asleep with medications for 3-6 hrs to observe for stability. While you are asleep you will be breathing with a breathing machine. The ICU specialist (Intensivist) is in charge of your care while you recover in the ICU. When you wake up you will feel very sleepy and weak. You will notice a few lines , tubes and wires connected to you which is routine. You will feel a bit uncomfortable with all those attached to your body. The additional lines are removed as you progress in your care and most are removed by day 5. As a routine, you will be helped to get out of bed and sit in a chair for a few hours to help your lungs breathe better. A physiotherapist will take you for a short walk on day 2 in the ICU. The stay in ICU is typically for 2 days. You will be transferred to the cardiac ward following this for further care.
Will I be in a lot of pain ?
Pain is very subjective but overall it’s uncommon for patients to experience severe pain. You will be given strong painkillers, some of which may have unpleasant side effects like nausea, vomiting and constipation. Nursing staff will manage your pain medication in close collaboration with you. You are encouraged to notify staff if your pain is unbearable, prevents you from deep breathing or keeps you awake.
Progress in ward
You will be in a room once you arrive in the ward. You will be connected to a monitor so nurses can see any alarming signals from your heart rhythm. You need to be careful that the wires remain attached to your body properly. If they get detached, you should inform your nurse by pressing the call button. The most important thing in the ward is to start getting more mobile. You will be asked to walk 5 times every day and your physio will teach you exercises. You may have some wires connected to you which will be removed after a few days. Removal of wires and lines are very tolerable. By day 5-7, you will be asked by physiotherapists to complete two flights of stairs. This is done to assess your fitness to be discharged home and your independent mobility. You will have regular blood tests and chest x rays. Electrolytes are frequently replaced with intravenous infusions.
Going home
Most patients are expected to be discharged between 5-7 days after minimally invasive surgery. You will receive discharge education from your nurse who will give you information about incisions, dressing, showering etc. A pharmacist will visit you to discuss your medications which might have changed a little bit. You must remember to take your discharge file with you that should include all your instructions regarding follow up appointments, a medication list and other material. You should carry this file with you when you visit your cardiologist or cardiac surgeon for follow up at 4-6 weeks.
Dressings
You will have a small dressing on the chest and one on the groin. You should remove it after 4 weeks under a running shower. You can remove it earlier if it starts to come off or breaks. If you have any concerns about the wound please visit your GP or notify Dr Joshi.
Follow up
You should arrange an appointment to see Dr Joshi in 6-8 weeks and your cardiologist in 8 weeks. You should visit your GP within a week after being discharged from hospital
Advantages of Hemisternotomy approach :
The anticipated advantages are reduced blood loss, shorter hospital stay and earlier return to activity. Half of the breastbone is kept intact which allows early resumption of activities.
- Cosmetic – incision is small and in some patients barely visible
- Early recovery and return to activities
- Future reoperations on heart are less complicated if you need one
- There may be less blood loss, shorter ICU and hospital stay
- Allows insertion of surgical valves which have the data of best long term performance compared to the one inserted from groin
Pictures :
Complications:
Generally considered a low risk operation despite the complexity associated with it. In the absence of major medical problems most patients have 1% or less risk of death or major complications. The most important complications to keep in mind are the risk of bleeding and stroke. Post operative bleeding is due to the requirement of delicate suturing in the high pressured part of the heart and stroke can result from any debris including blood clots blocking one of the vessels in the brain. The incidence of bleeding and stroke is expected to be around 1% and if the risks are higher it will be discussed at the time of consultation.
One of the important non major complications with this surgery is a risk of permanent pacemaker (PPM) which is about 5%.The valve is placed immediately next to your heart’s electrical system which may get compressed and malfunction. If your electrical system does not recover within a week then Mr Joshi will ask the cardiologist to insert a PPM under local anaesthetic prior to your discharge from hospital. Insertion of PPM does not hold you long in hospital or affect your recovery adversely.
Younger patients are a risk of developing fluid build up around the heart. This typically manifests at about 4 weeks. This is reactive fluid and younger patients are more prone. It is not harmful but can make some patients feel short of breath or feverish. If that happens you should present to ED or notify your cardiologist or Dr Joshi. The treatment involves anti-inflammatory medications and in some cases taking the fluid out with a needle or small incision.
Blood thinners ( warfarin or aspirin )
Duration and type of blood thinner depends on the type of valve that is implanted in the heart. If you have a tissue valve implantation then you will be on warfarin for 3 months and if you have a mechanical/metal valve then you will be on warfarin for life. When the surgery is elective, this will be discussed with you prior to surgery.
If you are fitted with a tissue valve then Dr Joshi or your cardiologist will advise when you are able to stop warfarin. Generally, warfarin is replaced with Aspirin 100 mg daily after 3 months.
What type of follow up after surgery?
Dr Joshi will see you for follow up after 6 weeks and then your long term follow up is organised by your cardiologist and GP. Echocardiogram is done once or twice a year to monitor the function of your heart and is done as seen necessary by your cardiologist. If you are on warfarin then your GP will guide you regarding frequency of blood tests and dosage of warfarin.
Will my life be normal after surgery?
One of the reasons to repair or replace your valve is to enable you to return to your normal life. If you have any limitations due to your heart issues then you should also get better, effectively improving the quality of your life. One would be expected to return completely back to normal life. However, if you are on warfarin or other blood thinners then necessary changes to your lifestyle are recommended.
Antibiotic prophylaxis prior to invasive procedures :
It is advised that you will need antibiotic prophylaxis for any future invasive procedure. You need to disclose to a treating practitioner or dentist about artificial prosthesis in your heart.
Right Anterior Thoracotomy Aortic Valve Replacement( RAT AVR)
What are the methods of Aortic valve replacement?
- AVR via full sternotomy( splitting breast bone)
- AVR via hemi sternotomy ( splitting 1/3rd of breast bone by incising on 3rd rib)
- AVR via right anterior thoracotomy ( breast bone is not divided at all)
- AVR via transfemoral route ( valve inserted via small incision in groin and no cuts on chest)
All the above methods of AVR are routinely employed. Except for AVR via full sternotomy the other three options are minimally invasive options for replacing the aortic valve. Not splitting breast bone(sternum) at all allows for quicker recovery, less blood loss, less hospital stay and better cosmesis.
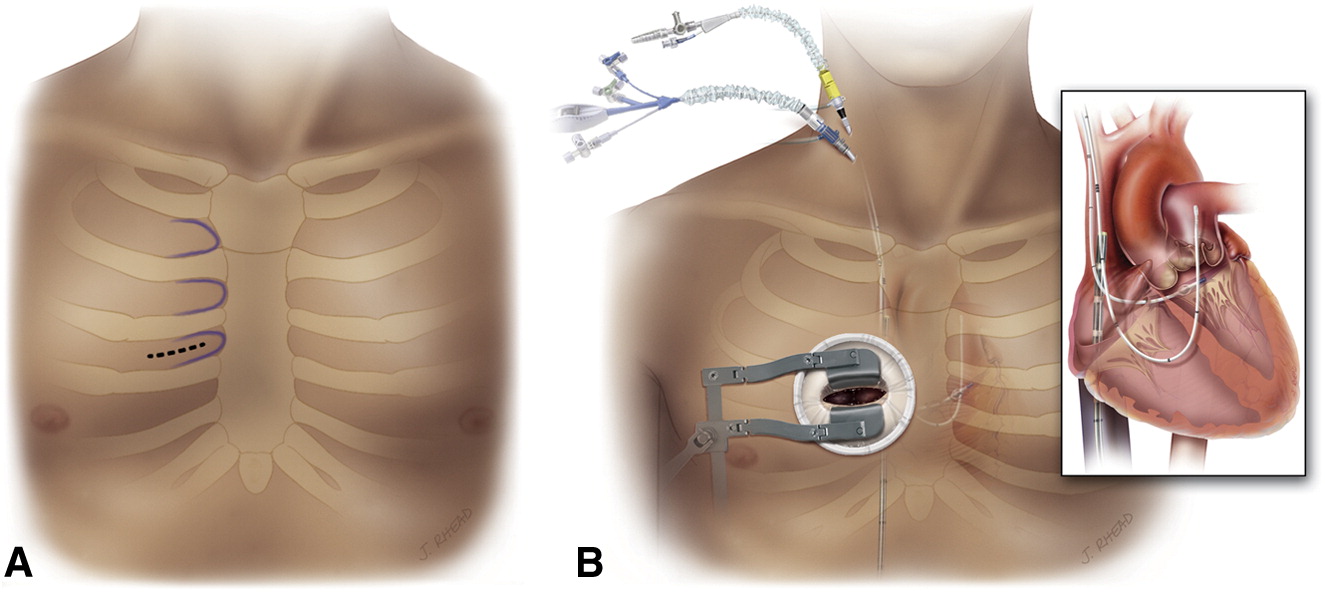
Right Anterior thoracotomy aortic valve replacement
This is a minimally invasive approach without touching the breastbone(sternum)
This operation is performed by a 5-7 cm incision on the right side of the chest. Entry into the chest is made by inserting a retractor in between the ribs. There is a 1 cm incision in the groin to connect the heart to the heart lung machine. The heart is stopped and protected with a special chemical solution. Aortic valve is replaced with biological/tissue or mechanical valve depending on the patient’s choice and circumstances. After inserting the valve all incisions in the heart and skin are closed and the patient returns to ICU for further stay for 1-2 days.
What happens in the ICU ?
Typically most patients are kept asleep with medications for 3-6 hrs to observe for stability. While you are asleep you will be breathing with a breathing machine. The ICU specialist (Intensivist) is in charge of your care while you recover in the ICU. When you wake up you will feel very sleepy and weak. You will notice a few lines , tubes and wires connected to you which are routine. You will feel a bit uncomfortable with all these attached to your body. The additionals are removed as you progress in your care and most are removed by day 5. As a routine, you will be helped to get out of bed and sit in a chair for a few hours to help your lungs breathe better. The physiotherapist will take you for a short walk on day 2 in the ICU. Stay in ICU is typically for 2 days. You will be transferred to the cardiac ward for further care.
Will I be in a lot of pain ?
Pain is very subjective but overall it’s uncommon for patients to experience severe pain. You will be given strong pain killers some of which may have unpleasant side effects like nausea, vomiting and constipation. Nursing staff will manage your pain medication in close collaboration with you. You are encouraged to notify staff if your pain is unbearable, prevents you from deep breathing or keeps you awake.
Progress in ward
You will be in a room once you arrive in the ward. You will be connected to a monitor so nurses can see any alarming signals from your heart rhythm. You need to be careful that the wires remain attached to your body properly. If they get detached, you should inform your nurse by pressing the call button. Most important thing in the ward is to start getting more mobile. You will be asked to walk 5 times every day and your physio will teach you exercises. You may have some wires connected to you which will be removed in the next few days. Removal of wires and lines are very tolerable. By day 5-7, you will be asked by physiotherapists to complete climbing two flights of stairs. This is done to assess your fitness to be discharged home and your independent mobility. You will have regular blood tests and chest x rays. Electrolytes are frequently replaced with intravenous infusions.
Going home
Most patients are expected to be discharged between 5-7 days after minimally invasive surgery like RAT AVR. You will receive discharge education from your nurse who will give you information about incisions, dressing, shower etc. A pharmacist will visit you to discuss your medications which might have changed a little bit. You must remember to take your discharge file with you that should include all your instructions regarding follow up appointments, medication list and other material. You should carry this file with you when you visit your cardiologist or cardiac surgeon for follow up at 4-6 weeks
Dressings
You will have a small dressing on the chest and one on the groin. You should remove it after 4 weeks under a running shower. You can remove it earlier if it starts to come off or breaks. If you have any concerns about wound please visit your GP or notify Dr Joshi
Follow up
You should arrange an appointment to see Dr Joshi in 6-8 weeks and your cardiologist in 8 weeks. You should visit your GP within a week after being discharged from hospital
Advantages of RAT approach :
Some of the advantages of the RAT approach is reduced blood loss, shorter hospital stay and earlier return to activity. The breastbone(sternum) is kept intact which allows early resumption of activities like lifting weight or driving.
- Cosmetic – incision is small and in some patients barely visible
- Early recovery and return to activities
- Future reoperations on heart are less complicated if you need one
- Less blood loss, shorter ICU and hospital stay
- Allows insertion of surgical valve which have the best records of long term performance compared to the one inserted from groin
Complications:
Generally considered a low risk operation despite complexity associated with it. In the absence of major medical problems most patients have 1% or less risk of death or major complications. Most important complication to keep in mind is the risk of bleeding and stroke. Post operative bleeding is due to the requirement of delicate suturing in the high pressured part of the heart and stroke can result from any debris including blood clots blocking one the vessels in the brain. The incidence of bleeding and stroke is expected to be around 1% and if the risks are higher it will be pointed out at the time of consultation.
One of the important non major complications with this surgery is a risk of permanent pacemaker (PPM) which is about 5%.The valve is placed immediately next to your heart’s electrical system which may get compressed and malfunction. If your electrical system does not recover within a week then Dr Joshi will ask the cardiologist to insert a PPM under local anaesthetic prior to your discharge from hospital. Insertion of PPM does not hold you long in hospital nor affects your recovery adversely.
Younger patients are a risk of developing fluid build up around the heart. This typically manifests at about 4 weeks. This is reactive fluid and younger patients are more prone. It is not harmful but can make some patients feel short of breath or feverish. If that happens you should present to ED or notify your cardiologist or Dr Joshi. The treatment involves anti-inflammatory medications and in some cases taking the fluid out with needle or small incision.
Chest wall hernia is one of the uncommon complications of this approach in which a part of the lung can protrude between your ribs at the site of incision. This is not a major complication but may need surgery in some patients.
Phrenic nerve injury is a very uncommon complication. Phrenic nerve is a nerve that supplies the breathing muscle on the right side of the lung. There is a possibility of its blood supply being damaged or injury to the nerve itself due to indirect traction during heart surgery.
Blood thinners ( warfarin or aspirin )
Duration and type of blood thinner depends on the type of valve that is implanted in the heart. If you have a tissue valve implantation then you will be on warfarin for 3 months and if you have a mechanical/metal valve then you will be on warfarin for life long. This would be discussed with you prior to surgery when it is elective.
If you are fitted with a tissue valve then Dr Joshi or your cardiologist will advise when you are able to stop warfarin. Generally, warfarin is replaced with Aspirin 100 mg daily after 3 months.
What type of follow up after surgery?
Dr Joshi will see you for follow up after 6 weeks and then your long term follow up is organised by your cardiologist and GP. Echocardiogram is done once or twice a year to monitor the function of your heart and is done as seen necessary by your cardiologist. If you are on warfarin then your GP will guide you regarding frequency of blood tests and dosage of warfarin.
Will my life be normal after surgery?
One of the reasons to repair or replace your valve is to enable you to return to your normal life. If you had any limitations due to your heart issues then you should also get better, effectively improving the quality of your life. One would be expected to return completely back to normal life. However, if you are on warfarin or other blood thinners then necessary changes to your lifestyle is recommended.
Antibiotic prophylaxis prior to invasive procedures :
It is advised that you will need antibiotic prophylaxis for any future invasive procedure. You need to disclose to a treating practitioner or dentist about artificial prosthesis in your heart.