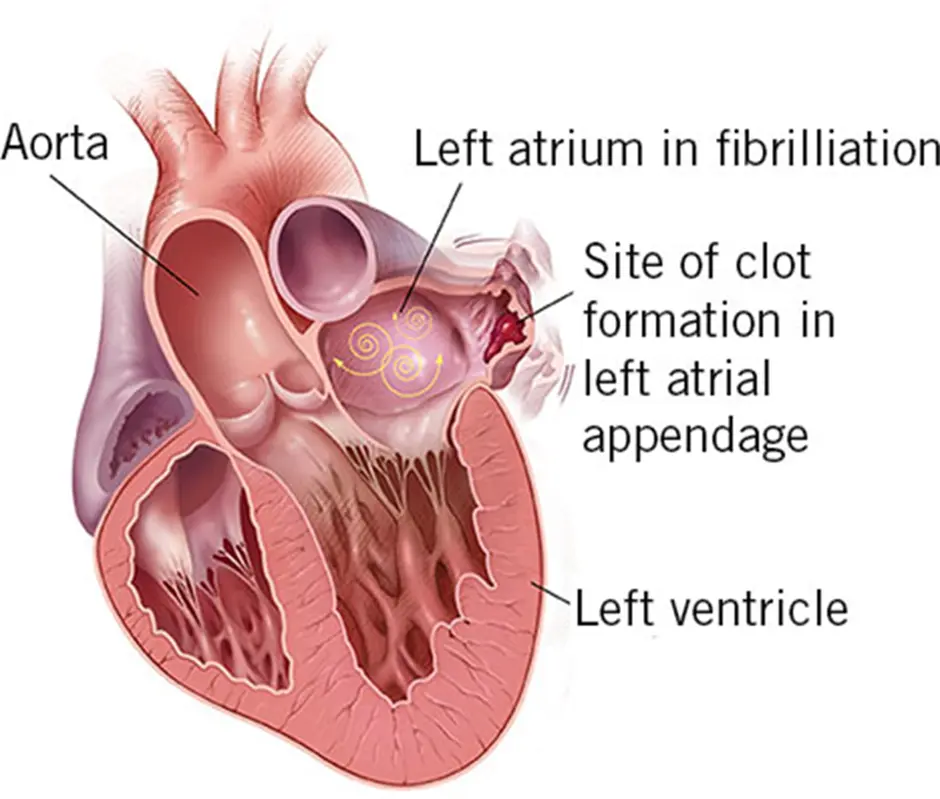
What is the left atrial appendage
Left atrial appendage is a small pouch on the left upper chamber of the heart. There is a similar pouch on the right upper chamber of heart. The main function of the pouch is to secrete a hormone that assists us in managing fluid balance in the body. Some believe that it also acts like a shock absorber if the chamber pressure rises.
How does the left atrial appendage cause stroke in patients with atrial fibrillation ?
In a normal heart rhythm, the left atrium (collecting chamber) contracts/pumps blood out of the atrium into the ventricle(pumping chamber). The left sided chambers pump blood to the entire body including the brain. Hence, blood is constantly moving through the heart chambers. In patients with the rhythm of atrial fibrillation, the left atrium stops pumping blood effectively leading to stasis of blood within the chamber. Blood passively flows through the heart in patients with atrial fibrillation. One of the drawbacks of blood stasis in the left atrial appendage is that it can form a blood clot. If the clot/thrombus escapes from the left atrial appendage it will travel into the left pumping chamber (ventricle) and the pumping chambers pumps the clot out of the heart into the body. If the clot lodges into the brain arteries it can result in a major stroke. If it lodges into arteries of any other organ it can cause detrimental effects.
How can one prevent clot/thrombus formation in left atrial appendage and prevent stroke ?
The most common way to prevent thrombus/clot formation is to start patients on stronger blood thinners that include warfarin. The newer, most common blood thinners are Xarelto, Eliquis and Pradaxa. Warfarin requires blood tests for monitoring while the newer agents do not require blood tests.Because of this,it is more convenient for patients and has become more popular. Blood thinners thin the blood and minimise the chances of clot formation in the appendage thus reducing the risk of stroke.
One of the side effects of blood thinners is excessive bleeding from minor injuries and in some patients life threatening bleeding episodes. Some patients can experience bleeding from their nose from blowing or bleeding from gums while brushing and these are considered minor bleeding episodes. Other patients can suffer from life threatening bleeding eg – bleeding from gut, urinary tract or brain. Being on blood thinners affects the lifestyle of active young people eg – sports, hiking etc.
Another way of stopping clot formation is to occlude the cavity of the left atrial appendage. As blood cannot enter the appendage after its occlusion, the clot formation in the appendage is prevented. This is achieved by placing a clip on the neck of the appendage and occluding the appendage. This method is a good alternative to blood thinners (anticoagulants)
Who is a candidate for thoracoscopic occlusion of left atrial appendage ?
- Patients with contraindications for blood thinners
- Patients who cannot take blood thinners reliably
- Patients in whom other means of occluding the appendage is not suitable
- Patients who are non compliant or do not want to take blood thinners
- Patients who are undergoing AF surgery
What are the other options other than Atriclip?
The left atrial appendage can be occluded with a device that is known as a Watchman device. It is inserted by a small puncture in the groin vessel, by the cardiologist. The cardiologist makes a puncture inside the heart to cross from the right side to the left side of heart. With the help of x-ray, a device that looks like an umbrella is inserted into the opening of the left atrial appendage. This device is anchored into its position with small barbs present on the outer surface of the device. It is advised that patients remain on anticoagulation (blood thinners) for 3-6 months as there is a chance of forming a blood clot on the device itself in the absence of blood thinners.
What is the difference between Atriclip and Watchman?
Atriclip is an externally placed device which is not in direct contact with blood while the Watchman is an internally placed device which is in direct contact with blood. No anticoagulation is necessary after insertion of Atriclip from the device point of view however, it is advised that patients stay on anticoagulation after insertion of Watchman device, as the device is in direct contact with the blood stream. Atriclip once placed doesn’t get dislodged, while there is a small chance of the Watchman device becoming dislodged, requiring urgent open heart surgery. Atriclip requires thoracoscopic procedures which is performed by 5 mm holes x 3 on the left chest while Watchman is inserted with a single puncture in groin. Both procedures require anesthesia and transesophageal echocardiogram to confirm appendage occlusion.