Thoracoscopic Lobectomy
Basics of Lung anatomy:

Thoracoscopic Lobectomy
Basics of Lung anatomy:
Lungs are breathing apparatus of human body. It has many functions but what it is mostly known for is breathing. The other functions of lungs include filtering particulate matter from air and charge immune system of body and work with heart in synchrony.
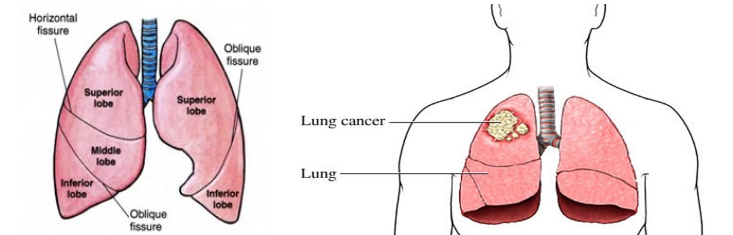
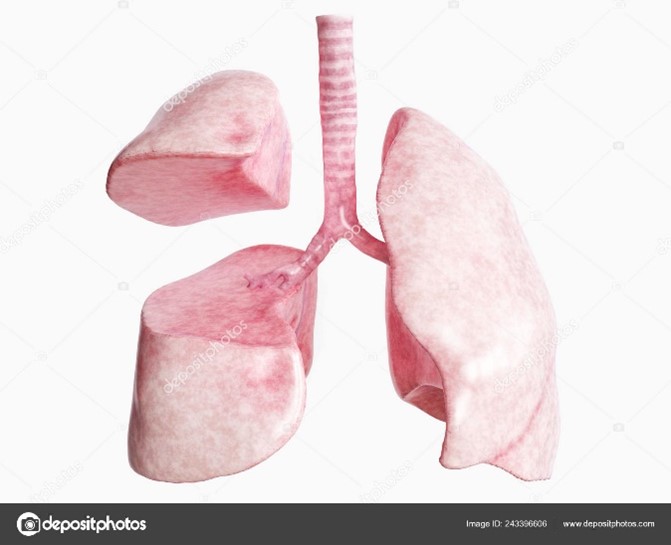
There are two lungs. Right lung has three divisions, and left lung has two divisions. The individual divisions are known as lobes. Each lobe has further subdivision which are not visible from outside which are known as segments.
Trachea is a breathing pipe which is also know is main airway. Airway (blue coloured pipe) is connected to both lungs as shown in diagram. It has two main divisions which are right and left. Both sides have further subdivisions for different segments of lung.
Each lobe is connected to its own division of airway, blood vessels routing deoxygenated blood into lungs and blood vessels routing oxygenated blood outside of lung.
What is lobectomy?
Lobectomy is a surgical removal of a lobe of lung. This is commonly done for resection of lung cancer. Other indications are infection or large bullae.
How is lobectomy performed?
There are three surgical approaches methods. All these approaches require general anaesthesia.
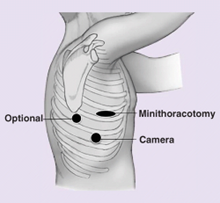
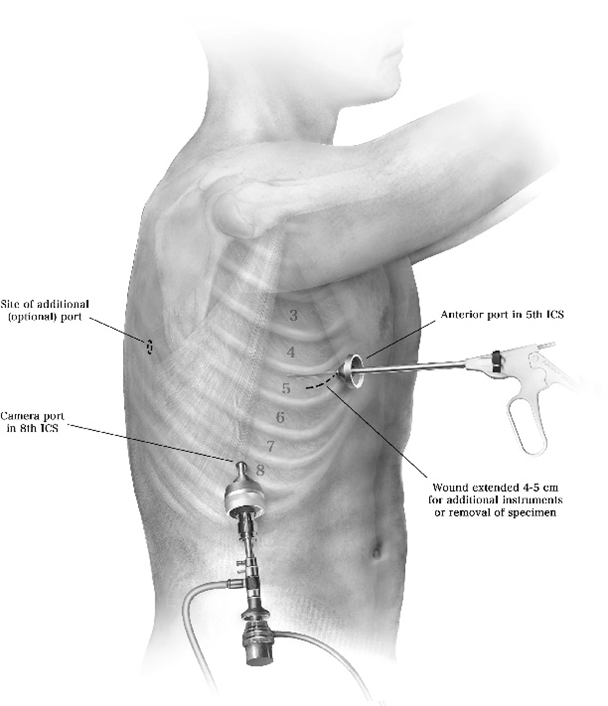
Thoracoscopic / VATS lobectomy
How is the lung divided or cut?
Surgeons use a special device that is known as surgical stapler (shown in picture). The stapler device is loaded with total of six rows of staplers. The device allows for lung tissue to be stapled where your surgeon wants to cut the lung. There is an inbuilt knife in the stapler device. The surgeon activates the knife which divides stapled lung tissues between 3 rows of staples on either side. This technology allows for tissues to not bleed and minimises the risk of air leakage from lung tissues. However, in patients with poor lung tissues(emphysema), the air can still leak from tiny holes caused by staples. Eventually these holes heal and stop leaking air. This is one of the reasons that the surgeon will leave a small drain coming out of your chest connected to drainage bottle. The drain is monitored on a regular basis for air and fluid leak. The drain is removed when Dr Joshi is happy with no air leaking.
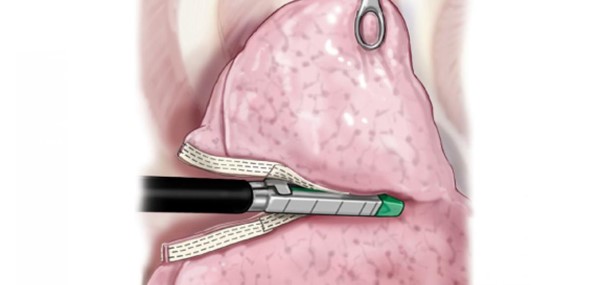
Stapler use for division of tissues.

Portable chest drain system displaying air leak and fluid drainage volume.
Will any Lymph glands be removed during surgery?
Removal of the lymph glands is very important with any cancer surgery and particularly with lung cancer operation. The human body has a rich network of lymph glands. Prior to surgery the lymph glands are assessed with a biopsy or PET Scan, however, there may be a small percentage of patients where cancer in the glands may be missed with these tests. To be sure, Dr Joshi will remove some lymph glands that are connected to the lungs. The presence of cancer cells in the lymph glands is considered as an advanced stage of cancer and may require chemotherapy for better control of cancer. Some patients are concerned about swelling in the arms or forearms which is not the case with removal of lymph glands for lung cancer surgery. Generally, there are no major side effects from removal of lymph glands but an occasional patient may develop lymph leak which may require further treatment.
After surgery the patient stays in recovery room until the anaesthetic wears off. After that the patient is transferred to the ward. Typically, the stay after surgery is expected to be between 2-3 days but some patients can go home after stay on 1 day if no air leak while some may need up to one week if there is an ongoing air leak in the drain. It takes about 2-3 weeks to become independent and get back to work. You should not drive for 2 weeks.

For the first two days, the most important thing that patients experience is pain from the operation and drains. Pain control methods include oral tablets, intravenous infusions and infusions around the spinal cord. Depending on the patient’s background history, the anaesthetist decides the pain control method. Some of the methods include a patient-initiated analgesia regimen which may include an infusion that patient can control,or on demand tablets for pain control.
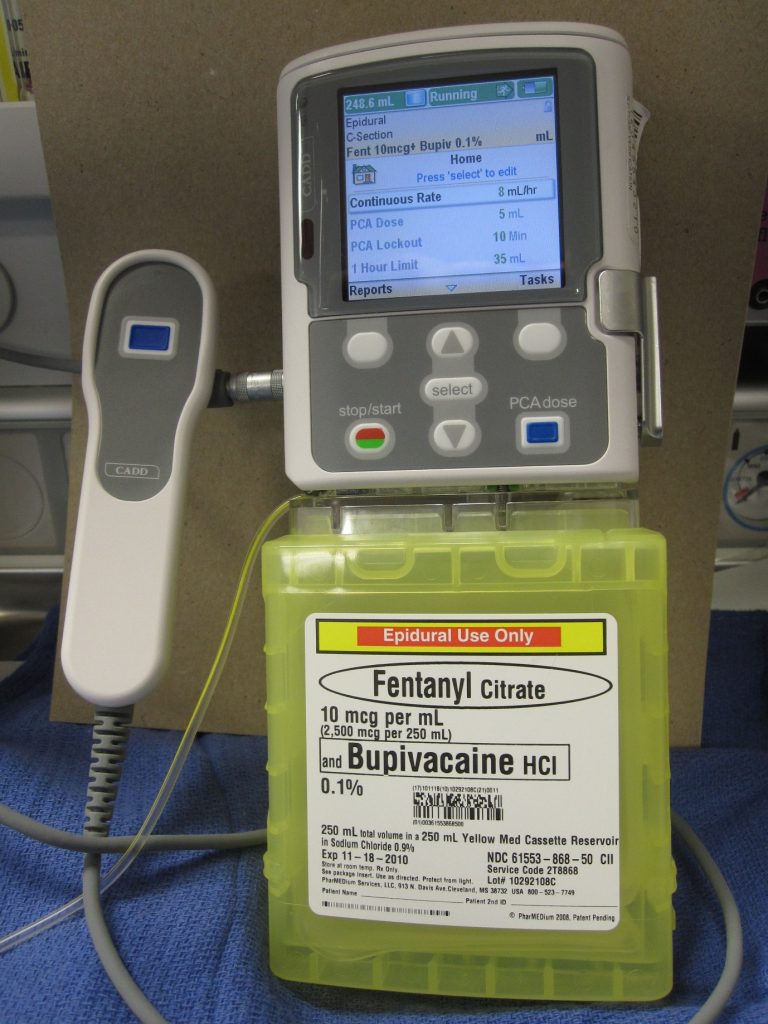
While recuperating in ward patients are visited by the physiotherapist. The patients are encouraged to participate in regular physiotherapy and mobilization. Apart from drains, patient is connected to an infusion system to control pain. It is quite cumbersome to move in and out of bed while drains and infusions are connected. Nursing staff will provide you with assistance. The patient can also call for staff if they want to move out of bed. Accidental disconnection of the drainage system or infusion can cause complications and its better avoided.
Your drain site has dressing on it. Occasionally it can stain with blood-stained fluid. You need to inform your staff. This is due to fluid collected in chest leaking around the drainage pipe. To experience this is uncomfortable but this is not a complication. Nurses may need change dressing frequently and will discuss with Dr Joshi. Dr Joshi will advise further course of action.
Dr Joshi will visit you on alternate days and his practice nurse will also visit you while you are in ward. The staff stays in regular communication with Dr Joshi about your progress. Your recuperation plan is guided by Dr Joshi. He will discuss with you regarding your discharge plan. Prior to you being discharged you will be given discharge instruction that includes
It is not uncommon to cough blood-stained phlegm for few days after surgery. It is due to surgical handling of airways during surgery. You should inform your surgeon but generally it subsides on its own.
You may experience fever in first 48 hours and your blood counts are expected to rise. This is not a sign of infection. However, if fever persists then some additional tests may be carried out and treatment will be commenced if infection is suspected.
Persistent air leak(PAL) – is one of the commonest complications and can occur in upto 10% of patients. If air leak persists more than 4 days then it is known as PAL. It is very rare for this to require further surgical treatment. Most patients have to stay in hospital until air leak stops. Rarely, Dr Joshi may need to perform VATS to identify air leak to treat this.
Subcutaneous emphysema – This is a relatively benign but most distressing complication for patients. It is an extension of air leak from lung surgery. For whatever reasons, if the leaking air is not removed by your drain then it starts to enter your fatty tissue and you will notice swelling of your skin over chest, chin, neck , forearms and eyes. The voice develops nasal twang. Most patients can feel crackling on their skin when they press their skin. If you note this on your body then it is very important to notify nursing staff quickly. They will ensure that your drain is not kinked or obstructed and notify Dr Joshi or his practice nurse for further advise.
Lung hernia – this is quite an uncommon complication and is seen in patients who develops coughing during recovery period. This usually is experience few weeks after surgery where patient experience bulge under the skin tissue during coughing or straining. This does not require surgery in most patients.
Nausea, vomiting and constipation are common side effects of pain medications and anaesthetic medications. Your staff will titrate the dose of pain medications for you to get optimum pain relief and to minimize side effects of pain medications. Pain does not completely disappear but the goal is to keep pain within the limit of tolerance and allowing for carrying out exercise and physiotherapy.
Infection of wounds, chest cavity and airway stump( divided end of airway) can occur however, very uncommon unless specific risk factors are present in patient (e.g. Patients on steroids, immunosuppressants, Diabetes, advanced cancer etc. )
Life threatening complications are very rare but worth noting. Heart attack can occur in patients with risk factors. Major bleeding can occur during surgery which may require converting key hole surgery to open surgery to be able to control bleeding. Patients who have cancers are at risk of developing blood clots in legs which has a risk of migrating to heart. Patients are given injections of weak blood thinner to prevent the occurrence of clots in legs.
One of the important long term side effects to note is nerve pain. With VATS surgery, the incidence of nerve pain is less likely however can occur. Nerves underneath each ribs are sensitive and delicate and can occasionally damaged while removing lung specimen. This will manifest as numbness over the front of chest or breast. Women may feel heaviness in breast. This side effects is likely to improve over period of time. Some patients may require pain killers.
The lobectomy specimen will be sent to Pathology lab. The pathologist performs detailed assessment of lung tissue and cancer. This can take upto 10 days. The pathology results are reviewed by specialist and may be presented in specialists meeting.
Will I be short of breath or require oxygen after lobectomy
Prior to surgery, Dr Joshi will organise lung function test to assess capacity of your lung. If your lung function tests are within the parameter to allow for lobectomy then only lobectomy will be performed. However, some patients may have suboptimal lung function. In these patients Dr Joshi will inform you about the potential side effects which may include being short of breath of exertion or having limitation in activity or physical capacity due to loss of lung tissue. Some patients can experience breathlessness or limitations despite normal lung capacity and this is very hard to predict prior to surgery. It is very rare for patients to require oxygen at home after lobectomy
Shall I stop smoking or vaping prior to surgery ?
It is most desirable that you stop smoking and vaping. Your risks of major complications including death will be high if you are a current smoker. Your recovery could be complicated by infection, cough and ICU stay.
If you are diagnosed with advanced lung cancer such as size more than 4 cm, presence of cancer cells in lymph glands or other high risk features then chemotherapy may be recommended. Dr Joshi will organise consultation with Medical oncologist. Radiotherapy is only considered if there is a suggestion of any cancer tissue left behind in the body due to difficult operation or technical issues due to location of cancer. This will be discussed with you if you need radiotherapy.
Dr Joshi or his practice nurse will organise review in his rooms at 3-6 weeks. You need to make an appointment to see your lung specialist or GP. After surgical review, you will be discharged back to your specialist who then will take over your care for future CT scans and surveillance to monitor cancer recurrence.