What is the Mediastinum ?
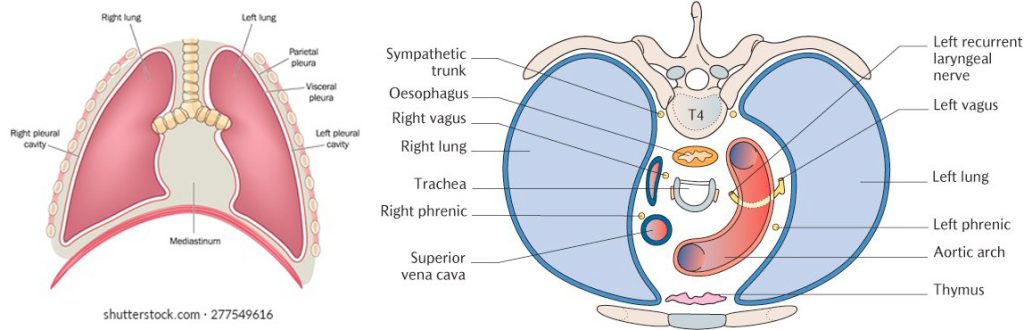
The mediastinum is a space in the chest cavity located between the two lungs. It contains the heart, blood vessels, nerves, glands, oesophagus, trachea and other internal organs.

What is the Mediastinum ?
The mediastinum is a space in the chest cavity located between the two lungs. It contains the heart, blood vessels, nerves, glands, oesophagus, trachea and other internal organs.
The mediastinum is divided into three compartments from front to back
It is also divided into two levels from neck to diaphragm
What is a mediastinal tumour?
A tumour is an excessive and abnormal growth of the tissues of various organs. It can be benign or malignant. Various organs can develop various different types of tumour.
What are the common mediastinal tumours?
Treatment
Different tumours require different types of approach. Some of the tumours can be treated with chemotherapy and radiotherapy while some are best treated with surgical excision.
Surgical excision can be done with an open approach that requires splitting of the sternum(breastbone) or thoracotomy (Large incision on chest wall that involves spreading ribs). The other approach is a minimally invasive approach, also known as “ keyhole surgery”. Large tumours are best approached with an open approach while small tumours can be removed with minimally invasive surgery.
VATS excision of tumour
VATS (Video assisted thoracoscopic surgery) excision of tumour is done under general anaesthesia. The patient is fully asleep and does not feel sensations or pain. Special anaesthetic techniques are used that allows the surgical team to allow for controlled collapse of the lung on the side of surgery.
Dr Joshi makes 1 cm incisions which varies between 3-4. Carbon dioxide is introduced in the chest cavity to allow for adequate space for surgery to be carried out. Visualization of the surgical field is obtained by the introduction of a telescope. Various types of specialised instruments are used to separate the tumour from vital structures. Once the tumour is separated, Dr Joshi makes another incision just under the ribs to remove the tumour outside of the chest cavity. A small tube is left inside the chest cavity to remove any collected blood or fluid during surgery. The tumour is sent to the pathology lab for further examination. The patient is woken up after surgery and transferred to the recovery room or ICU
After surgery the patient stays in the recovery room until the anaesthetic wears off. After that the patient is transferred to the ward. Typically, the stay after surgery is expected to be between 2-3 days. It takes about 2 weeks to become independent and get back to work. You should not drive for 2 weeks.

For the first two days, the most important thing that patients have to deal with is pain from the operation and drains. Pain control methods include oral tablets, intravenous infusions and infusions around the spinal cord. Depending on the patient’s background history the anaesthetist decides the pain control method. Some of the methods include a patient initiated analgesia regimen which may include infusion that patient can control or on demand tablets for pain control.
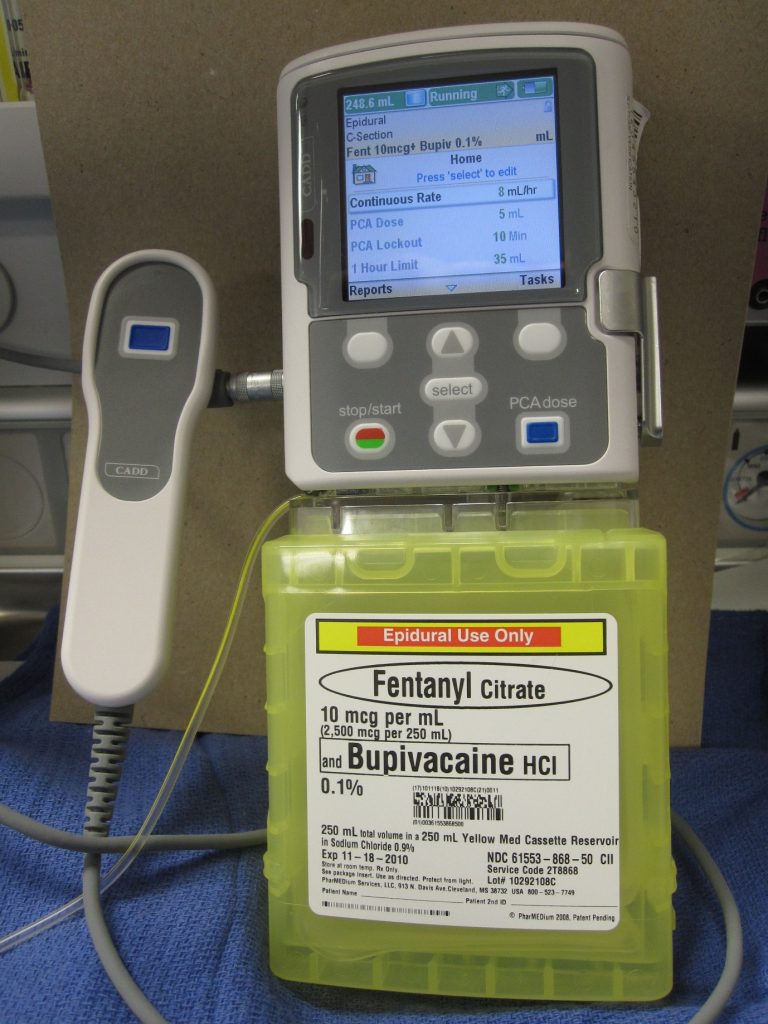
While recuperating in the ward patients are visited by a physiotherapist. The patients are encouraged to participate in regular physiotherapy and mobilization. Apart from drains, patients are connected to an infusion system to control pain. It is quite cumbersome to move in and out of bed while drains and infusions are connected. Nursing staff will provide you with assistance. The patient can also call for the staff if they want to move out of bed. Accidental disconnection of the drain system or infusion can cause complications and it’s better avoided. Drains are usually removed the next day.
Your drain site will have a dressing on it. Occasionally it can stain with blood-stained fluid. You need to inform your staff. This is due to fluid collected in the chest leaking around the drainage pipe. Site of fluid leakage can be uncomfortable but this is not a complication. Nurses may need to change dressings frequently and will discuss with Dr Joshi. Dr Joshi will advise further course of action.
Dr Joshi will visit you on alternate days and his practice nurse will also visit you while you are in the ward. Staff stay in regular communication with Dr Joshi about your progress. Your recuperation plan is guided by Dr Joshi. He will discuss with you regarding your discharge plan. Prior to you being discharged you will be given discharge instruction that include:
It is not uncommon to cough blood-stained phlegm for a few days after surgery. It is due to surgical handling of the airways during surgery. You should inform your surgeon but generally it subsides on its own.
You may experience a fever in the first 48 hours and your blood counts are expected to rise. This is not a sign of infection. However, if fever persists then some additional tests may be carried out and treatment will be commenced if infection is suspected.
Nausea, vomiting and constipation are common side effects of pain medications and anaesthetic medications. Your staff will titrate the dose of pain medications for you to get optimum pain relief and to minimize side effects of pain medications. Pain does not completely disappear but the goal is to keep pain within the limit of tolerance and allow you to carry out exercise and physiotherapy.
Infection of wounds and chest cavity can occur however, this is very uncommon unless specific risk factors are present in patient (e.g. Patients on steroids, immunosuppressants, Diabetes, advanced cancer etc. )
Mediastinum houses some of the important structures including nerves. Injury to these structures is rare but worth noting. Some of the tumour requires dissecting tissues close to the phrenic nerve that supplies the diaphragm (breathing muscle).Damage to this nerve can lead to paralysis of this nerve which may result in shortness of breath which may require future interventions. Recurrent laryngeal nerve supplies voice box and injury to this nerve can lead to hoarseness of voice. Injury to the thoracic duct can lead to accumulation of fatty fluid in the chest that requires complex management.
Life threatening complications are very rare but worth noting. Heart attacks can occur in patients with risk factors. Major bleeding can occur during surgery which may require converting keyhole surgery to open surgery to be able to control bleeding. Patients who have cancers are at risk of developing blood clots in legs which have a risk of migrating to the heart. Patients are given injections of weak blood thinner to prevent the occurrence of clots in legs.
One of the important long term side effects to note is nerve pain. With VATS surgery, the incidence of nerve pain is less likely however it can occur. Nerves underneath each rib are sensitive and delicate and can occasionally be damaged while removing lung specimens. This will manifest as numbness over the front of the chest or breast. Women may feel heaviness in their breasts. These side effects are likely to improve over a period of time. Some patients may require painkillers.
Dr Joshi will arrange a post operative review in his rooms between 3-4 weeks. This is to assess your wounds, chest x-ray and discuss the results of examination of your lung specimen. After that he will discharge you to your referring doctor and GP.
You will be under follow up with your referring doctor who will inform you of a follow up plan that may include regular CT scan of chest.
Dr Joshi will discuss your results in the Multidisciplinary Team meeting(MDT). Experience has shown that participation in MDT is likely to improve a patient’s long term outcome. MDT consists of your surgeon, referring lung specialist, oncologist (cancer specialist), radiologist and radiation oncologist (specialist of radiotherapy). Combined opinion is sought and recommendation is made by the team which benefits your long term outcome. If the tumour is cancerous then you may be referred to a medical or radiation oncologist for further treatment.
Most patients are expected to return back to normal life. There are no restrictions on activities a few weeks after VATS. However, there may be some restriction on activity after an open approach for a few weeks. Depending on the type of tumour, some patients may require long term treatment or surveillance.