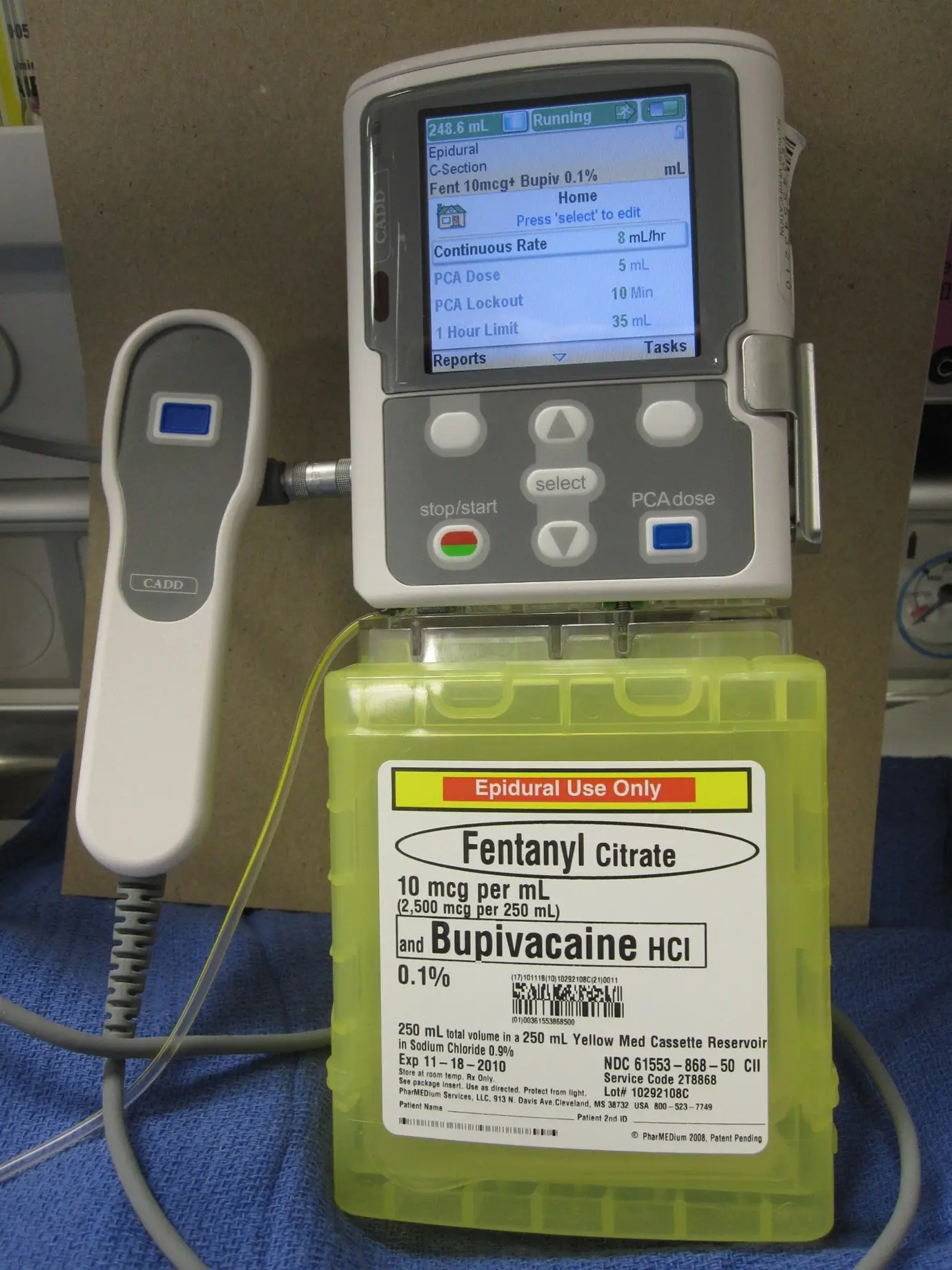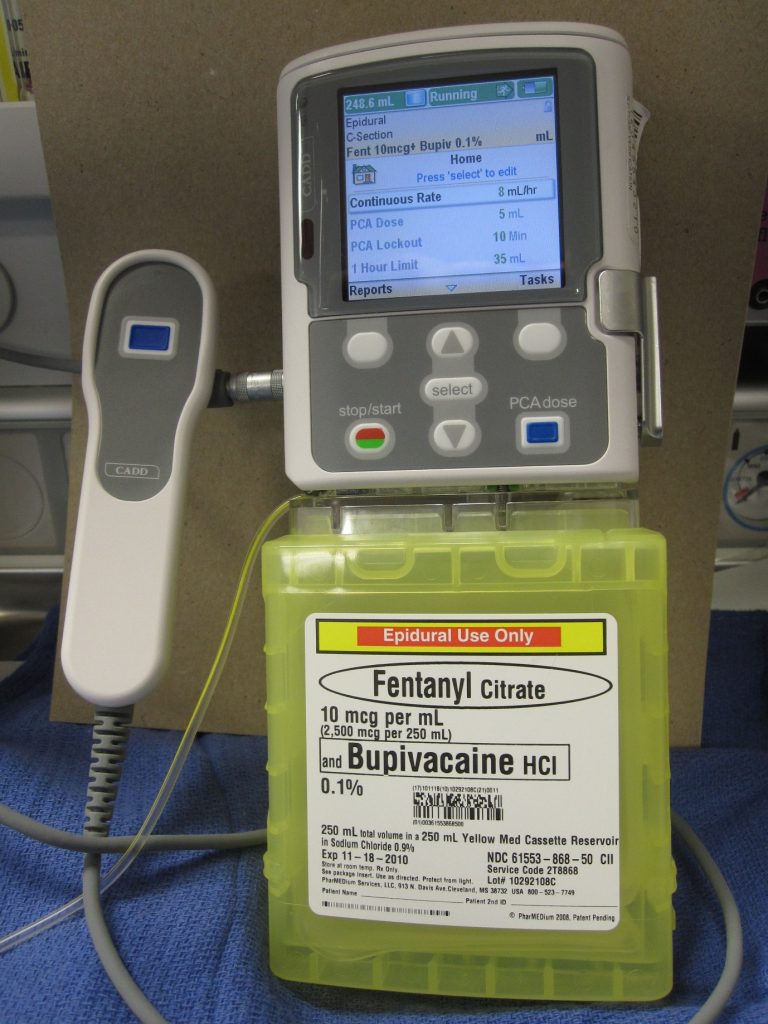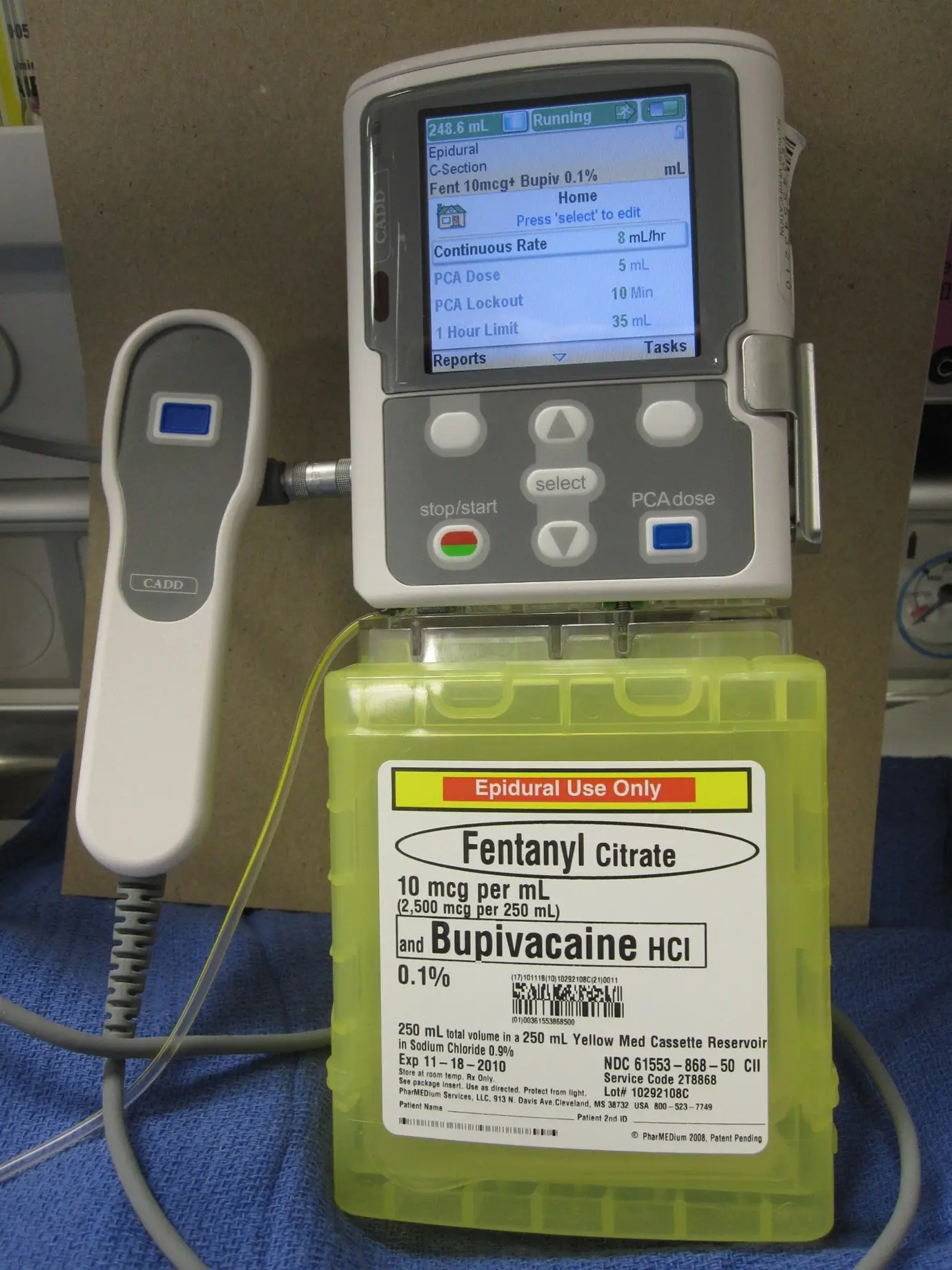
Figure: Patient controlled analgesia infusion system
While recuperating in ward patients are visited by physiotherapist. The patients are encouraged to participate in regular physiotherapy and mobilization. Apart from drains, patient is connected with infusion system to control pain. It is quite cumbersome to move in and out of bed while drains and infusions are connected. Nursing staff will provide you with assistance. The patient can also call for the staff if they want to move out of bed. Accidental disconnection of drain system or infusion can cause complications and its better avoided. Drains are usually removed next day.
Your drain site has dressing on it. Occasionally it can stain with blood-stained fluid. You need to inform your staff. This is due to fluid collected in chest leaking around the drainage pipe. Site of fluid leakage can be uncomfortable but this is not a complication. Nurses may need change dressing frequently and will discuss with Dr Joshi. Dr Joshi will advise further course of action.
Dr Joshi will visit you on alternate days and his practice nurse will also visit you while you are in ward. The staff stays in regular communication with Dr Joshi about your progress. Your recuperation plan is guided by Dr Joshi. He will discuss with you regarding your discharge plan. Prior to you being discharged you will be given discharge instruction that includes
- Discharge letter
- Instruction for removal of sutures and dressings
- Advise regarding care of wounds and how to seek medical attention or advise in case of any potential complications.
- Advise regarding making appointment with Dr Joshi, your referring specialist and GP
Complications
It is not uncommon to cough blood-stained phlegm for few days after surgery. You should inform your surgeon but generally it subsides on its own.
You may experience fever in first 48 hours and your blood counts are expected to rise. This is not a sign of infection. However, if fever persists then some additional tests may be carried out and treatment will be commenced if infection is suspected.
Nausea, vomiting and constipation are common side effects of pain medications and anaesthetic medications. Your staff will titrate the dose of pain medications for you to get optimum pain relief and to minimize side effects of pain medications. Pain does not completely disappear but the goal is to keep pain within the limit of tolerance and allowing for carrying out exercise and physiotherapy.
Infection of wounds and chest cavity can occur however, very uncommon unless specific risk factors are present in patient (e.g. Patients on steroids, immunosuppressants, Diabetes, advanced cancer etc.)
Life threatening complications are very rare but worth noting. Heart attack can occur in patients with risk factors. Major bleeding can occur during surgery which may require converting key hole surgery to open surgery to be able to control bleeding. Patients who have cancers are at risk of developing blood clots in legs which has a risk of migrating to heart. Patients are given injections of weak blood thinner to prevent the occurrence of clots in legs.
One of the important long term side effects to note is nerve pain. With VATS surgery, the incidence of nerve pain is less likely however can occur. Nerves underneath each ribs are sensitive and delicate and can occasionally damaged while removing lung specimen. This will manifest as numbness over the front of chest or breast. Women may feel heaviness in breast. This side effects is likely to improve over period of time. Some patients may require pain killers.
Treatment after VATS diaphragm plication
Dr Joshi will arrange post operative review in his rooms between 3-4 weeks. This is to assess your wounds, chest x ray and discuss the results of examination of your lung specimen. After that he will discharge you to your referring doctor and GP.
You should avoid lifting heavy weight and avoid exertional work for 6 weeks.
Life after VATS diaphragm plication
After 6 weeks you should be able to return back to normal life. Sometimes despite good early results failure can occur. It depends on tissue quality and strain placed on repaired diaphragm after surgery.