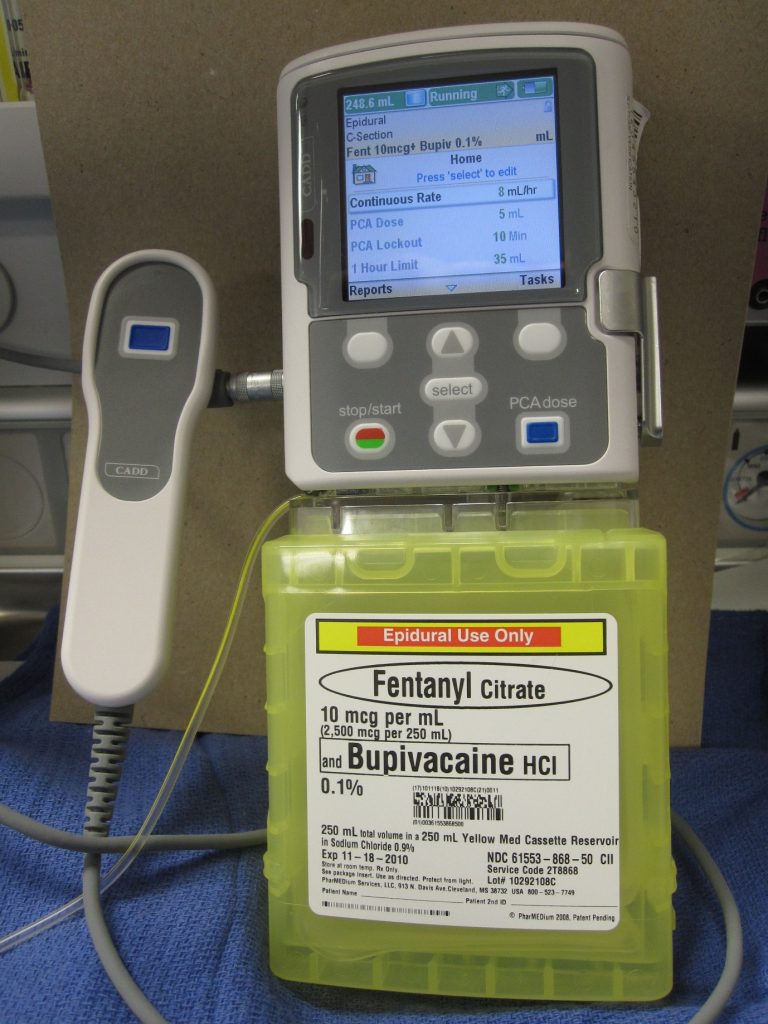
For the first two days, the most important thing that patients have to deal with is pain from the operation and drains. Pain control methods include oral tablets, intravenous infusions and infusions around the spinal cord. Depending on the patient’s background history the anaesthetist decides the pain control method. Some of the methods include a patient initiated analgesia regimen which may include infusion that patient can control or on demand tablets for pain control.
Figure : Patient controlled analgesia infusion system
While recuperating in the ward patients are visited by a physiotherapist. Patients are encouraged to participate in regular physiotherapy and mobilization. Apart from drains, patients are connected to an infusion system to control pain. It is quite cumbersome to move in and out of bed while drains and infusions are connected. Nursing staff will provide you with assistance. The patient can also call for the staff if they want to move out of bed. Accidental disconnection of the drain system or infusion can cause complications and it’s better avoided. Drains are usually removed the next day.
Your drain site has a dressing on it. Occasionally it can stain with blood-stained fluid. You need to inform your staff. This is due to fluid collected in the chest leaking around the drainage pipe. The site of fluid leakage can be uncomfortable but this is not a complication. Nurses may need to change dressings frequently and will discuss with Dr Joshi. Dr Joshi will advise on a further course of action.
Dr Joshi will visit you on alternate days and his practice nurse will also visit you while you are in the ward. Staff stay in regular communication with Dr Joshi about your progress. Your recuperation plan is guided by Dr Joshi. He will discuss with you regarding your discharge plan. Prior to you being discharged you will be given discharge instructions that include:
- Discharge letter.
- Instruction for removal of sutures and dressings.
- Advice regarding care of wounds and how to seek medical attention or advice in case of any potential complications.
- Advice regarding making an appointment with Dr Joshi, your referring specialist and GP.