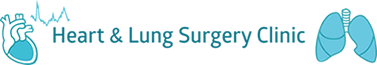
The chest cavity has many organs but the biggest organs in the chest are the lungs. The lungs are full of air that we breathe in and out. Lungs are like balloons in a box. Air can go inside the balloon but it does not leak outside the balloon into the box. If air continues to leak from the balloon into the box without any outlet then air will accumulate and collapse the balloon. Similarly, if there was a puncture or tear on the surface of the lung, air that we breathe in gets out of the lungs and accumulates in the chest cavity between the chest wall and the lungs. If we don’t let this air out then it causes lungs to collapse resulting in breathing difficulty, and death sometimes. The medical term for this condition is “Pneumothorax” ( Pneumo = air, thorax = chest cavity)
Pneumothorax (collapsed lung)

What are the causes of pneumothorax?
- Primary pneumothorax – the lungs are essentially normal but there are some weak areas which are called blebs or bullae. They break open like a ruptured blister and cause air to leak.
- Secondary pneumothorax- in this condition there is usually some underlying lung condition that leads to a tear in the surface of lung causing pneumothorax.
Other causes for pneumothorax are post trauma/accident, post lung biopsy and in women with endometriosis.
How is pneumothorax treated?
- Observation – not all pneumothorax require surgical treatment. Small and asymptomatic pneumothorax can be treated with observation. It may require serial x-rays.
- Insertion of chest drain – In patients who are symptomatic or have a total collapse of lungs, the air from the chest cavity is drained with needle aspiration or insertion of a soft rubber chest drain to evacuate air.
- Surgery – This is done for patients who have more than one episode of pneumothorax or have a high likelihood of recurrent pneumothorax. It is also done for patients who continue to leak air as seen by bubbles leaking out of chest drains. The other reasons for offering surgery depends on patient factors like previous life threatening episodes, patients living away from metropolitan areas, pilots or high risk professionals.
What is the surgery for Pneumothorax ?
Surgery for pneumothorax is known as pleurodesis.
The purpose of pleurodesis is to create adhesions between the chest wall and the lungs. Therefore if a patient develops future episodes of pneumothorax, lung collapse can be minimised. Most surgeons also try to identify areas of the lung with weakness/bleb/bullae and remove it with surgical staples to minimise future recurrence.
What does the surgery for pleurodesis involve?
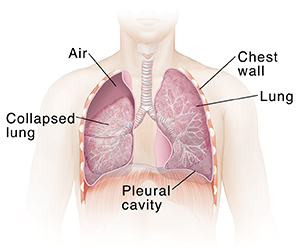
Surgery is done with a minimally invasive approach utilizing key holes and telescope assistance, which is known as Video Assisted Thoracoscopic Surgery (VATS). The other approach involves thoracotomy which has some disadvantages compared to VATS (hyperlink to difference between VATS and Thoracotomy approach)
VATS pleurodesis is done under general anaesthesia meaning that the patient is fully asleep and does not feel any pain/sensation or be aware of the operation. The anaesthetist uses a specialised technique that allows for patients to breathe via the lung that is not being operated on. Urinary catheterization is not generally used. However, if patients fail to pass urine after surgery then catheterization may be necessary.
Duration of surgery is generally less than 30 mins for the surgical part. The time for delivery of anaesthesia and preparation for surgery adds another 40 mins prior to surgery. Patients are woken up straight after completion of surgery. There is a drain inserted on the side of the operation. The purpose of the drain is to remove any fluid or blood that may have collected during surgery and also to remove any fluid or air after surgery.
Surgery involves 2 x 1 cm incisions and a third 3 cm incision on the chest wall. After introducing the telescope Dr Joshi will inspect the lungs and chest wall. After identification of the weakened area of the lung, he removes it with surgical staples. Surgeons use surgical staplers to divide the lobe from the rest of the lungs. The stapler uses 3 rows of fine titanium staples to seal the division of lungs. Following this pleurodesis is achieved with spraying medical talc or removing the inner membrane
(Parietal pleura) of chest wall which is known as pleurectomy. The purpose of this is to cause inflammation which assists in creating adhesions between the chest wall and the lung to prevent future collapse.
When a patient starts to breathe from the side of the operated lung, he/she starts to breathe air on that side. Some of the air can leak from the holes created by the row of staples. The majority of them seal straight away but sometimes it can take longer for the tiny holes to seal. If this air is not evacuated by placement of drain then the air accumulates in the chest and collapses the lung. So, one of the most important purposes of drain is to remove air that may leak from the staple hole after lung resection surgery. Most surgeons will remove drains in 6-24 hrs after the air leak has stopped.
After surgery the patient stays in the recovery room until the anaesthetic wears off. After that the patient is transferred to the ward. Typically, the stay after surgery is expected to be between 2-4 days. It takes about 2-3 weeks to become independent and get back to work. You should not drive for 2 weeks.

For the first two days, the most important thing that patients have to deal with is pain from the operation and drains. Pain control methods include oral tablets, intravenous infusions and infusions around the spinal cord. Depending on the patient’s background history the anaesthetist decides the pain control method. Some of the methods include a patient initiated analgesia regimen which may include infusion that patient can control, or on demand tablets for pain control.
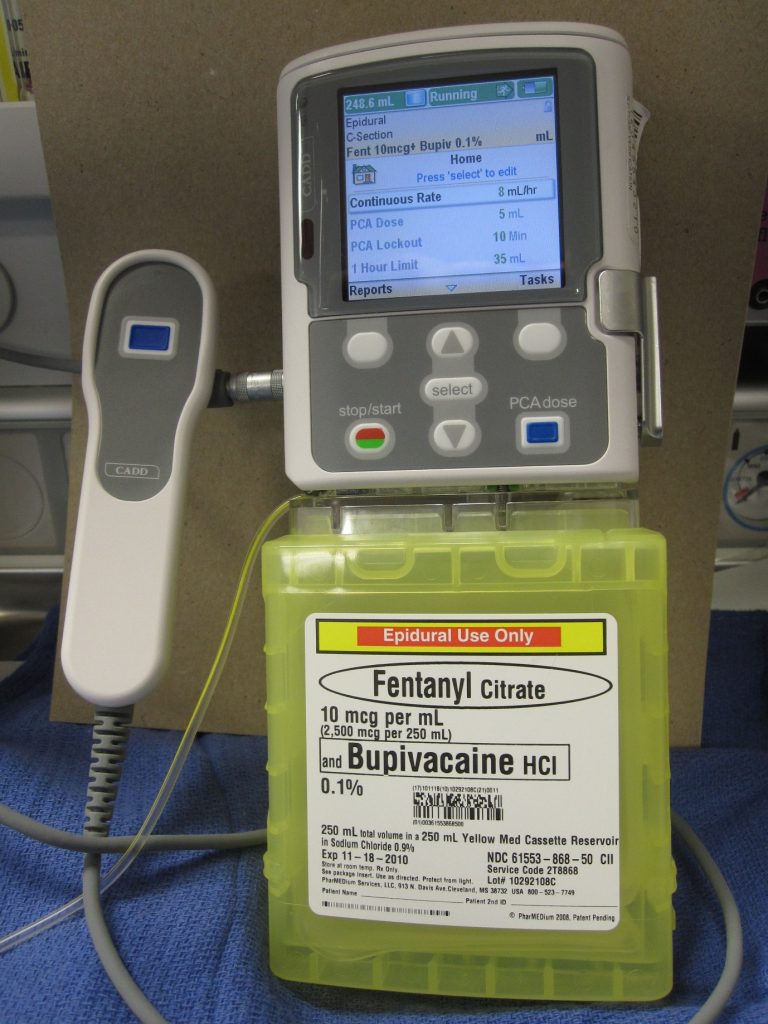
Figure : Patient controlled analgesia infusion system
While recuperating in the ward patients are visited by a physiotherapist. The patients are encouraged to participate in regular physiotherapy and mobilization. Apart from drains, patients are connected to an infusion system to control pain. It is quite cumbersome to move in and out of bed while drains and infusions are connected. Nursing staff will provide you with assistance. The patient can also call for the staff if they want to move out of bed. Accidental disconnection of the drain system or infusion can cause complications and it’s better avoided.
Your drain site has a dressing on it. Occasionally it can stain with blood-stained fluid. You need to inform your staff. This is due to fluid collected in the chest leaking around the drainage pipe. To experience this is uncomfortable but it is not a complication. Nurses may need to change dressings frequently and will discuss with Dr Joshi. Dr Joshi will advise on a further course of action.
Dr Joshi will visit you on alternate days and his practice nurse will also visit you while you are in the ward. The staff stay in regular communication with Dr Joshi about your progress. Your recuperation plan is guided by Dr Joshi. He will discuss with you regarding your discharge plan. Prior to you being discharged you will be given discharge instruction that includes
- Discharge letter
- Instruction for removal of sutures and dressings
- Advise regarding care of wounds and how to seek medical attention or advise in case of any potential complications.
- Advise regarding making appointment with Dr Joshi, your referring specialist and GP
It is not uncommon to cough blood-stained phlegm for a few days after surgery. This is due to surgical handling of the airways or lungs during surgery. You should inform your surgeon, but generally it subsides on its own.
You may experience a fever in the first 48 hours and your blood counts are expected to rise. This is not a sign of infection. However, if fever persists then some additional tests may be carried out and treatment will be commenced if infection is suspected.
Nausea, vomiting and constipation are common side effects of pain medications and anaesthetic medications. Your staff will titrate the dose of pain medications for you to get optimum pain relief and to minimize side effects of pain medications. Pain does not completely disappear but the goal is to keep pain within the limit of tolerance and allow for carrying out exercise and physiotherapy.
Infection of wounds, chest cavity and airway stump (divided end of airway) can occur however, it is very uncommon unless specific risk factors are present in patient (e.g. Patients on steroids, immunosuppressants, Diabetes, advanced cancer etc. )
Life threatening complications are very rare but worth noting. Heart attacks can occur in patients with risk factors. Major bleeding is very unlikely in this operation. Patients are at risk of developing blood clots in the legs which have a risk of migrating to the heart. Patients are given injections of weak blood thinner to prevent the occurrence of clots in legs.
One of the important long term side effects to note is nerve pain. With VATS surgery, the incidence of nerve pain is less likely however it can occur. Nerves underneath each rib are sensitive and delicate and can occasionally be damaged while removing lung specimens. This will manifest as numbness over the front of the chest or breast. Women may feel heaviness in their breasts. This side effect is likely to improve over a period of time. Some patients may require painkillers.
You will be advised at the time of discharge for follow up. It is not always necessary to follow up with Dr Joshi in his rooms. However, if you wish to see him please notify the ward staff to book an appointment at the time of discharge or call his rooms. If you arrange to visit Dr Joshi’s rooms then you will need a chest x-ray 1 week prior.
You should visit your GP after your discharge from hospital. You will be discharged with drain sutures which will need to be removed at your GP practice after 5-7 days. You should arrange a review with your referring specialist.
If Dr Joshi has removed the weak portion of the lung, it is sent to the Pathology lab for examination. The results will be sent to your referring doctor.
One of the common worries most patients have is whether they will be able to breathe normally and get back to their normal life. In this surgery the portion of the lung that is removed is very small and unlikely to affect your breathing. Patients who have borderline lung function tests are likely to experience breathing problems long term but Dr Joshi will discuss this with you prior.
Most patients are able to resume their normal life, activity and exercises after about 4 weeks. Your exercise capacity will continue to improve with time. There are restrictions on some activity after pleurodesis and you should discuss this with your specialist. If you are a deep sea diver, then you need to consult a respiratory specialist for fitness especially if you had VATS pleurodesis instead of thoracotomy (recurrence rate of pneumothorax are slightly higher – up to 10%). Professional pilots and long distance train drivers should also discuss with their specialist about their fitness to return back to their profession.