What type of patients:
- Patients with leaking aortic valves
- Patients with swollen (dilated) aorta affecting aortic valve
Who does surgery:
This is done by surgeons who have significant experience in doing this surgery. Your heart surgeon needs special training to be able to do this surgery. He also needs to have an experienced team that includes an anaesthetist who is able to assess your valve before and after your repair to ensure that a good result has been obtained. To maintain the skill and good outcome, your surgeon and his team should be doing this surgery on a regular basis.
Tests before surgery:
Dr Joshi will organise a special preparation CT scan of your entire aorta. You may have had a scan done prior to seeing him but he will need to request a special scan to further assess the feasibility of this operation. The second test that he may organise is known as TOE (Transesophageal echocardiogram). This test is done by a cardiologist which Dr Joshi will organise. This test is meant to assess the repairability of your valve. With this information Dr Joshi can better plan your surgery and also inform you prior to surgery about the probability of repairing the valve successfully.
Apart from above tests, other routine tests prior to heart surgery involve blood tests, x-ray and some other tests which will be done before or after you are admitted to hospital.
About the Surgery:
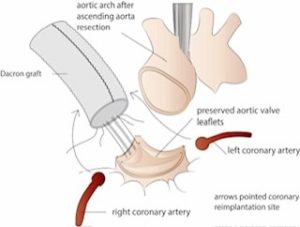
This surgery usually takes longer than other usual heart surgeries. The operation can last up to 5 hrs. If your aorta needs to be replaced then Dr Joshi will use one of the commercially available artificial tubes (Figure 1) made from Dacron cloth which is designed to last life long. He may have to use a commercially available ring to reshape your repaired valve. Sometimes to repair a leaflet he may use a patch made from a harvested pig heart to reconstruct one of the leaflets . He removes the unwanted aorta and leaves your valve attached to its skeleton. He then stitches your valve back into the new tube. He checks the valve is geometrically symmetrical and assesses again with intraoperative echo prior to separating you from the heart lung machine. In rare cases, the repaired valve does not function well and in that case Dr Joshi will replace your valve with a pre decided tissue or mechanical valve.