What does this operation involve ?
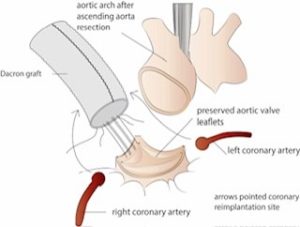
As the name suggests in this operation,aneurysmal Aortic root is replaced with sparing of the native aortic valve. In conventional aortic root replacement surgery, aortic root replacement includes replacement of the ascending aorta , aortic root and aortic valve with reimplantation of coronary arteries. In VSARR , everything is similar to conventional aortic root replacement, except that instead of an artificial valve,the patient’s own aortic valve is used.
What are the advantages of VSARR over conventional aortic root replacement ?
VSARR is very similar to conventional aortic root replacement except that the patient’s own aortic valve is retained instead of replacing it with a mechanical or tissue valve. All artificial valves expose patients to an additional lifetime risk of stroke and infection . Mechanical valves have an added lifetime risk of bleeding while tissue valves may require future interventions. Patient’s native valves have a lower risk of the complications associated with artificial valves.
Am I a candidate for VSARR ?
Not everyone is suitable for VSARR. The native valve should be in good condition and anatomically suitable for reimplantation. Some patients are born with two leaflets instead of three but they can still have this operation as long as their leaflets are in good condition. The risk of failure increases if it is done in patients who are not suitable for VSARR. The surgeons who are experienced (more than 30 operations in their career) will advise you whether you are a suitable candidate for VSARR. To assess your candidacy for this operation your surgeon will organise a CT scan and transoesophageal echocardiogram after assessing your initial investigations.
What are the indications of VSARR ?
Typically this operation is done in patients who have an aortic root aneurysm with relatively normal structure of the aortic valve. Very experienced surgeons also perform this operation in patients with an acute tear in the aortic root. This operation is not suitable for patients with aortic root aneurysm with calcified aortic valve leaflets.